Living with High Cholesterol
You have been diagnosed with high cholesterol levels, and you would like to know the basics about this condition, as well as understand what it means for you?
High cholesterol
Why get checked ?
Cholesterol is a global chronic disease
Am I at risk of high cholesterol?
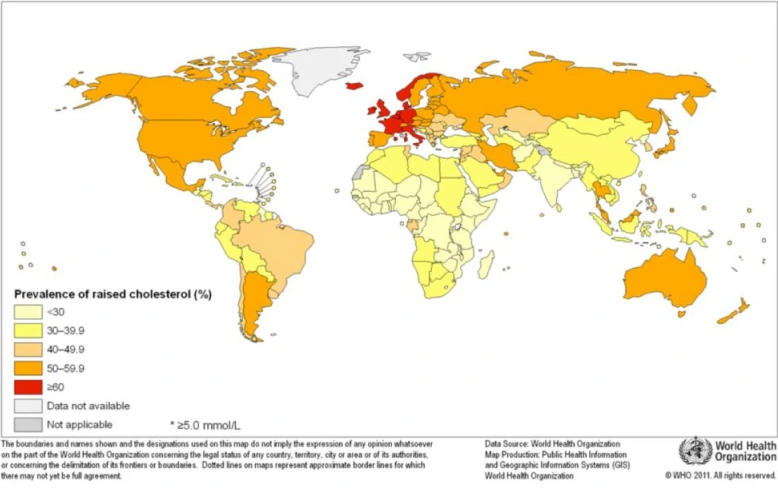
Hypercholesterolemia is a very common condition. In 2008, the World Health Organization published statistics regarding the prevalence of raised total cholesterol among adults worldwide.1
Many risk factors have been identified for high cholesterol.
Age
The risk for hypercholesterolemia increases with age. Because the body’s capacity to clear cholesterol deteriorates as we get older, cholesterol levels increase, which in turn raises the risk of stroke and heart disease.2
Gender
Until their mid-50s (or until menopause), women tend to have lower bad cholesterol levels, and at any age higher good cholesterol levels. Still, after menopause (around age 55), LDL cholesterol levels in women increase.2,3
Family history
Some forms of hypercholesterolemia can be due to the overproduction of bad cholesterol by the liver, with a genetic predisposition. In many cases, though, high cholesterol stems from a combination of genetics and diet, for family members often share behaviors and lifestyles.2
Behaviors and lifestyle choices
The different levels of blood tests results
I have seen HDL and LDL on my blood results. How should I interpret them?
Cholesterol tests require a blood draw, indeed, but a lipid profile features more than just HDL and LDL. Your test results also show your triglyceride level, and the total cholesterol level.
Triglycerides are a type of fat that is an energy resource for the body, and total cholesterol represents the total amount of cholesterol in blood, entailing HDL, LDL, and triglycerides.
In an adult, desirable cholesterol levels are as follows:
Triglycerides are a type of fat that is an energy resource for the body, and total cholesterol represents the total amount of cholesterol in blood, entailing HDL, LDL, and triglycerides.
In an adult, desirable cholesterol levels are as follows:
Generally desirable level
Total cholesterol
under 200 mg/dL or 5.2 mmol/L
LDL (bad) cholesterol
under 100 mg/dL or 2.6 mmol/L
HDL (good) cholesterol
under 60 mg/dL or 1.5 mmol/L
Triglycerides
under 150 mg/dL or 1.7 mmol/L
Your results are important, but they should be interpreted by your physician. Depending on your age, gender, family history, your lifestyle, your smoking habits (or lack thereof), and other cardiovascular risk factors, your physician will be able to understand the full picture and determine whether action should be taken or not, if high LDL cholesterol levels should be lowered.4
Indeed, some drugs can increase LDL or triglyceride levels. Among those, one can mention glucocorticoids, some diuretics, oral estrogens, and b-blockers.2
Indeed, some drugs can increase LDL or triglyceride levels. Among those, one can mention glucocorticoids, some diuretics, oral estrogens, and b-blockers.2
Level changes can be influenced by many factors
Why have my cholesterol levels gone up since my last test?
Many factors can come into play, when it comes to high cholesterol levels. Among other things, one can mention age (the risk for hypercholesterolemia increases with age), lifestyle choices, including food habits or a lack of exercise, weight gain, or even the use of some medications.5,6
Cholesterol check frequency
How often do I need to get my cholesterol checked?
Cholesterol levels should be tested at least every 4 to 6 years starting at age 20, and more often if you have a family history of high cholesterol. Talk to your doctor about what’s right for you.5
Before a blood test
Will I need to do anything to prepare for the cholesterol test?
You may need to fast–no food or drink–for 9 to 12 hours before your blood is drawn. Your health care provider will let you know if you need to fast and if there are any special instructions to follow.7
Are there any risks to the cholesterol test?
Don’t worry, there is very little risk to having a blood test. You may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly.7
References
6
Rhee EJ, Kim HC, Kim JH, et al. 2018 Guidelines for the management of dyslipidemia. Korean J Intern Med. 2019;34(4):723-771.